My Fertility Journey

I have hummed and hawed a lot about whether I want to write about my fertility journey on this blog, so publicly, open for anyone to see. But I know that when I was going through it, blog posts like this really helped me to feel less alone, so that is my impetus.
Guess what – we’re pregnant!
Wow, once it is happening it is so easy to just be in that moment. The months of struggle and sadness slowly fading away.
When we got pregnant with our daughter in January 2018, we were just about to start fertility treatment. So, deciding to try and conceive for the second time, we suspected it wasn’t going to be a quick journey. In fact, now we were that much older, and I was that much further away from having had my laparoscopic surgery for endometriosis, so I suspected things would only be harder. Yet, there was a shred of hope that maybe, just maybe, my body would remember what to do and just pick it up easier this time. No such luck.
About six months into trying to conceive, I decided to start looking into at least getting on a fertility clinic wait list, knowing there was a pretty good chance we were going to end up needing these services. Luckily, I have an amazing friend / colleague / mentor who helped me to get in with Dr. Hannam at Hannam Fertility in Toronto. Him and his Nurse Carly were both wonderful to work with.
We had originally been told that we would likely get a call for IVF in the spring of 2021 (we were on the funded cycle list). In January (this is now 12 months into TTC), we got a call that they had some funding left from the previous year and did we want to start the process basically….right away. I know for some people doing IVF right at the 12 month mark is unusual. Especially since I never even tried IUI. But having some level of background knowledge in this fertility world, I knew my best chances for success were with IVF, and frankly, I just wanted to get this show on the road. We knew we only wanted two children, and the age gap between our first and second wasn’t getting any smaller.
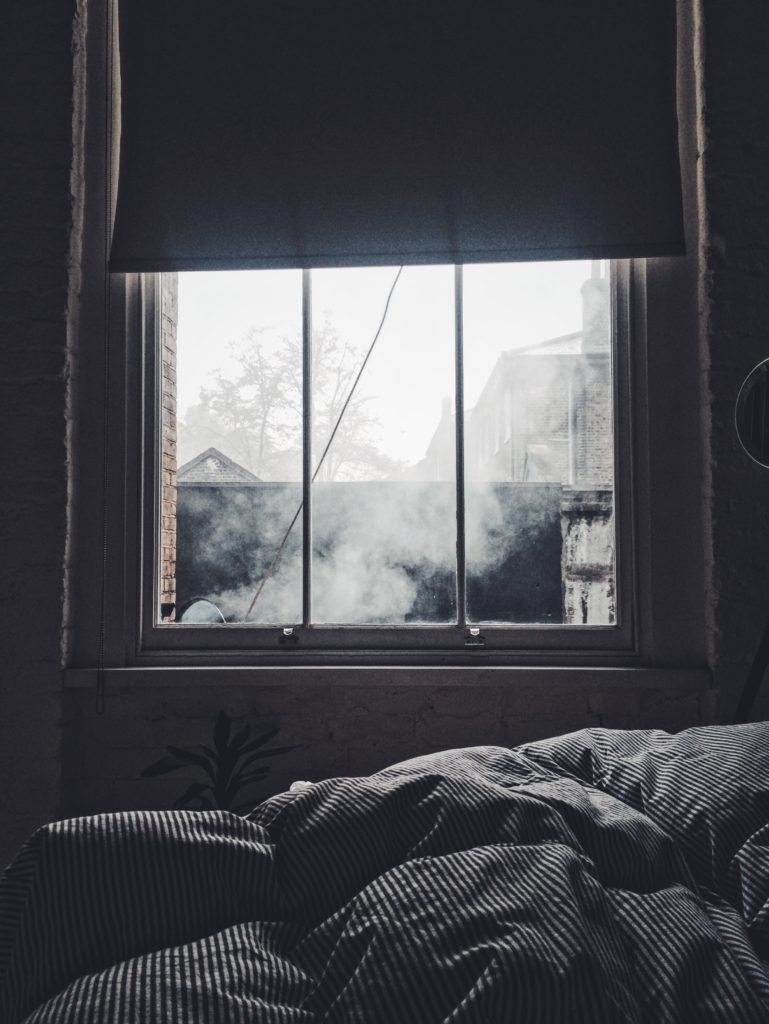
February 1, 2021 was my first day driving into Toronto for an appointment. The first part of several small fortunes spent on medication, blood work and ultrasound done. Let the process begin! Being a Registered Nurse and Naturopathic Doctor, the medication process wasn’t too challenging for me. Sure, injecting yourself with a needle everyday (sorry make that two needles) is nerve wracking at first, but you get used to it pretty quickly. Some days the side effects sucked (like day after day of headaches), and some days were fine.
By March 11, 2021, we were ready for egg retrieval. Having a low AMH, I was told I probably wouldn’t get a lot of eggs. So, the whole team was pleasantly surprised when we got 16 eggs! However, as time went on, the numbers diminished. Only 9 of those eggs matured, only 5 of them fertilized, and only ONE embryo survived to day 5. I knew I wasn’t going to do this process over again, so it was very disheartening to know we only had one shot. Our embryo was graded 4AB, which is pretty good and our doctor was happy with this embryo. Meanwhile, after the egg retrieval, I got a mild case of OHSS (ovarian hyperstimulation syndrome), which meant pain while moving, twisting, and not being able to fit into your clothing. During this time I was congratulated on my pregnancy, which really was the icing on the cake.
Between March and June I got to take a bit of a break and then started preparing my body for our transfer. On June 7, 2021 (which happens to be my Mom’s birthday) we went back to Toronto for our embryo transfer. Patrick wasn’t allowed to come into the space with me (thank you COVID!), but we FaceTimed with him so he got to observe the whole process. It was an exciting and happy day. After the transfer the painful part is the w a i t i n g. June 15 was the day I went for my blood test to find out if I was pregnant. People often say “when you relax you will get pregnant”. Well, let me tell you, I was not relaxed, not once, during that waiting period. I was an anxious, nervous wreck, who felt like time was going in reverse. I swear it was the longest 8 days of my entire life.
I guess you know where this story goes next….it worked! Our one little miracle embryo decided to stick around! And now we are just waiting for him to make his grand appearance in February 2022.
This story is leaving lots of things out – all the various emotions, the many other drives to Toronto, missing work, the financial stress, the physical toll, navigating questions from people around if you want to have a second child…..and so much more. Something I really found challenging was making career choices during this time. When you never know how long it will take you to conceive, it can be hard to decide what career moves you want to make. Knowing that MAYBE a big (mat leave) career break will be coming, or maybe it never will. Also, questioning if you really want two kids. Maybe you only want one? Maybe you are okay with being a family of three? Or maybe you are just telling yourself that so that you don’t feel sad? The emotions all get very confusing and muddled and sometimes the journey just feels never ending.
Of course I know we had it WAY way easier than lots of folks going through infertility. We only went through the IVF process once. But hey, it still wasn’t a walk in the park. I feel blessed beyond all measure that we have this baby on the way. I also feel relief knowing I never have to try to conceive again. I feel relief knowing my body will be all mine again. I feel fortunate that I have friends, family and colleagues who were all so supportive during this time. Every fertility story is unique, but if you are going through the process, I hope you found at least one thing here helpful.